Phenethylamine crops up in some of the more interesting chapters of organic chemistry’s history. It traces roots back to 1876, when Ernst Von Meyer isolated it from natural sources. Early chemists noticed its presence in plants and animals, including the human brain, giving rise to the idea that certain bodily experiences trace back to these amines. By the mid-20th century, researchers closely tracked its chemical cousins: amphetamines and compounds like dopamine. These explorations changed the way we think about neurotransmitters, the connections between mood and chemistry, and the role trace amines play in things like energy, motivation, and perception. That historic curiosity drives many current research trails, both in academic labs and in fields circling back to traditional medicine.
Pure phenethylamine usually turns up as a colorless, oily liquid or sometimes as crystal-like solids at cooler temperatures. It slides into various roles: dietary supplement, chemical intermediate, and research tool, showing up in everything from over-the-counter brain boosters to advanced chemical syntheses. In commercial settings, production scales up to deliver clean, high-purity material for the food sector, the pharmaceutical pipeline, and even niche perfume houses crafting scents that call on musky, floral, or green top notes.
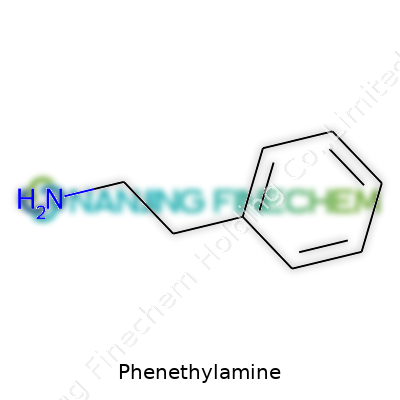
Phenethylamine’s formula is C8H11N; the structure reveals a benzene ring tacked onto a short ethylamine chain. It boils near 195°C, melts just under 0°C, and dissolves well in water and organic solvents—alcohol, ether, and others. Its basic character rides on the amine group. In air, it picks up a faint fishy scent. Its simple core forms the backbone for endless modifications, morphing into compounds with radically different biological effects, all hinging on tweaks to the side chains or ring substitutions.
Regulators step in to manage phenethylamine’s sale and labeling. Bottles list precise purity levels, often 99% or higher for research or industrial-grade batches. Safety data appears up front: hazard ratings, storage rules, and recommended handling gear. Suppliers provide certificates of analysis, MSDS forms, and sometimes extra documentation showing low levels of residual solvents, heavy metals, and contaminants. For supplement use, labels warn consumers about potential mood or stimulant effects, sometimes pointing out interactions with medications or health conditions. In my own workplace, I’ve seen strict chain-of-custody processes that chase every gram from warehouse to workbench, especially where local laws flag phenethylamine under precursor controls or industrial poisons.
Synthesis often follows a reductive amination route. Chemists start with benzaldehyde, mixing it with ammonia or a primary amine, kicking off a reaction that, with a hydrogen donor and catalyst like palladium on carbon, yields phenethylamine. Sometimes, they favor reduction of phenylacetonitrile with lithium aluminum hydride or catalytic hydrogenation for bulk operations. These routes aim for clean conversion, skimming off byproducts and controlling side reactions that spawn unwanted tars or off-smelling residues. Industrial setups wrap these syntheses in closed reactors, vent lines, and monitoring systems, not just for quality but to keep fumes and accident risks in check.
Chemists see phenethylamine as a versatile platform. Alkylation bolts on longer carbon chains, shifting how the molecule interacts with neurons or enzymes. Nitration seeds the ring for further reduction or rearrangement, spawning useful intermediates. Many designer drugs borrow this skeleton, tweaking it to modulate psychoactivity, pharmacokinetics, or safety. Pharmaceutical firms look at halogenation, hydroxylation, and acylation to sharpen selectivity or dial down toxicity. In real terms, anyone handling phenethylamine in the lab must mind its reactivity: oxidation can create quinones and colored impurities, so storage and handling call for dry, cool, airtight containers. Simple missteps can turn a benign experiment into a set of bitter lessons.
Phenethylamine shows up under a web of different names depending on context: beta-phenylethylamine, 2-phenylethylamine, or PEA. On chemical supply lists, you might spot designations like NSC 12432 or UN 2676. Supplement brands often label it just as PEA, but pharmaceutical circles will lean on stricter INCI or CAS numbers—CAS 64-04-0. In some old research, it appears as phenylethanolamine or by the chemical formula itself. These aliases sometimes cause confusion, especially for regulators or buyers sorting through a crowded marketplace.
Direct exposure to concentrated phenethylamine brings short-term risks: eye or skin irritation, breathing difficulty with big spills, or mild toxicity if swallowed. Safety standards in labs demand gloves, splash goggles, and fume hood work. National and international regulations—OSHA, REACH, GHS—classify the compound under hazardous chemicals, and every drum comes with signage. Shipping follows UN 2676 rules, and waste disposal must track local environmental laws. In my experience, even seasoned chemists respect the unpredictability of amines: accidental mixing with oxidizers or acids triggers swift, sometimes violent, reactions.
Phenethylamine’s reach stretches well beyond the lab. It serves as a starting point for antidepressants and weight loss drugs, a natural stimulant in energy supplements, even a chemical intermediate for dyes and surfactants. Brain chemistry research singles it out as a model for studying trace amines—the lesser-known siblings to dopamine or serotonin. In forensic science, it pops up as an analyte; analysts look for its presence in biological samples to screen for use of banned stimulants. Food technologists trial it for modulating flavor releases, though most applications circle back to small-scale specialty uses instead of bulk food manufacturing.
Research into phenethylamine keeps gaining ground. Its role as a neurotransmitter or neuromodulator makes it a hot ticket in studies of depression, ADHD, and even Parkinson’s disease. Scientists build libraries of analogs, each new variant inching closer to better efficacy and fewer side effects than older antidepressants or stimulants. Pharmaceutical development aims to refine selectivity: tightening receptor targets, cutting down risk of neurotoxicity, and skipping unwanted cardiac stimulation. Some recent papers discuss phenethylamine’s odd link with endurance and athletic performance, sparking new lines of inquiry for sports medicine and wellness entrepreneurs.
Toxicology teams test phenethylamine in rodent and cell studies, watching for acute and chronic harms. Overdosing in animals stokes hyperactivity, anxiety, and cardiovascular stress, but doses similar to those found in chocolate or dietary supplements prove far milder. Long-term exposure data lags behind, so regulatory authorities steer on the cautious side, suggesting limits for supplemental intake and requiring clear risk disclosures. While some anecdotal users report mood boosts, headache and insomnia also show up post-use, especially with high, repeated intake. Medical researchers want deeper, multi-year studies, particularly on how PEA interacts with psychiatric or cardiac meds.
Looking ahead, phenethylamine occupies a curious crossroads. Drug designers keep revisiting its chemical backbone aiming for new ways to treat mental health disorders. The supplement sector sees marketing opportunities in compounds “found in chocolate,” though consumer advocates push for tighter oversight. Synthetic biology experiments explore plant-based production of trace amines, which lowers process hazards and environmental impact compared to full-scale petrochemical syntheses. Personal experience in the field shows me how quickly regulatory winds can shift: one year, a compound is just another research tool; next year, it’s flagged for misuse or tightly controlled. Long term, clear labeling, robust toxicology, and transparent sourcing will matter more than ever, as interest in trace amines and their analogs keeps climbing and the line between supplement and medicine grows thinner.
Phenethylamine pops up in places a lot closer than you’d think. It flows through chocolate, hiding behind that little mood boost many claim to feel after a bite. It hangs out in supplements with bold promises on the label. It’s a compound people seem to stumble over in both science labs and nutrition stores. The reason it shows up so often has to do with what it does in our brains and bodies.
Our brains already know what phenethylamine is. We make it naturally, and it acts a bit like an internal stimulant. Think about dopamine – the chemical we hear about when learning, enjoying things, or feeling alert. Phenethylamine helps trigger some dopamine release. Some scientists call it a “trace amine,” meaning our bodies don’t flood with it, but we need it in just the right spots.
There’s the everyday stuff: a good laugh, a burst of creative energy, the rush after a brisk walk. These can shake loose a little more phenethylamine inside us. Researchers have measured those spikes, often linking them to improved mood or motivation.
Step into a health shop or scan supplements online, and phenethylamine capsules won’t be tucked away. They usually land in blends that aim to sharpen focus, cut appetite, or boost mood. The appeal makes sense – the push to lift your energy for a big meeting or chase away a morning fog. Companies market it for these reasons, and folks chasing that edge give it a shot.
Trouble shows up when appetite for these effects runs wild. Adding phenethylamine to your day without careful thought can tangle things up, especially if other stimulants already play a part. Headaches, anxiety, and racing heartbeats are real risks. Several countries have taken note and set limits for how much can go into supplements. One country’s borders might block a shipment that another lets through without a care.
Pharmaceutical researchers haven’t let phenethylamine pass by. They tinker with its structure, building medicines used in everything from nasal decongestants to treatments for attention problems. Amphetamines, which treat ADHD, borrow heavily from the phenethylamine backbone. It’s a skeleton key for unlocking a host of drugs used in psychiatry and neurology. None are over-the-counter for a reason – they pack a real punch, so doctors watch doses closely.
Chocolate keeps cropping up in phenethylamine talk. Some claim it’s the magic behind feeling better after a chocolate binge. Science offers a mixed picture. While this compound is found in cocoa, your body digests it pretty quickly and doesn't let much slip into the brain. Still, many people don’t need a reason to smile about chocolate, and phenethylamine adds to the sweet mystery.
No one compound solves all our problems. Phenethylamine looks exciting in a lab, but what matters shows up in daily life. It’s easy to hope that a pill might wipe away low energy or sadness, but real changes often come from steadier habits: good sleep, a balanced diet, regular movement, some time with people we care about. If mood and motivation keep dropping, or focus slips for months, that’s when a chat with a doctor helps much more than rolling the dice on another supplement.
With all the interest around phenethylamine, more research remains on the table. Scientists piece together how it works, where it helps, and where to draw the line. As for me, a square of chocolate and a walk outside usually brighten the day just fine.
Some folks are curious about phenethylamine, a compound found in chocolate and sold at vitamin shops. The internet can sell anything, and this one comes dressed up in promises: better mood, sharper focus, maybe even weight loss. Just because it shows up in chocolate bars doesn’t mean sprinkling it into your morning coffee makes sense.
I grew up watching people reach for quick fixes—energy drinks, mood boosters, pills with barely pronounceable names. Phenethylamine gets attention because it’s tied to dopamine, that "feel good" brain chemical. The catch: when you swallow phenethylamine, your body breaks most of it down in minutes. Very little gets to your brain, and what little does probably disappears before you even notice anything.
Science tries to dig deeper. Researchers point out that phenethylamine shares some chemistry with amphetamines. Some experiments found a boost in alertness. But no major health organization calls it a magic cure or recommends it for brain fog, depression, or attention issues.
Head to a health food store and you’ll see phenethylamine bottles by the checkout register, sometimes next to herbal sleep aids or bodybuilding boosters. No one behind the counter screens for health issues, sensitive heart rhythms, or mental health struggles.
Plenty of people think, “It’s natural, I saw it in a list of ingredients, it must be fine.” But that approach leads folks into trouble. Stimulant effects—racing heart, blood pressure spikes, anxiety—have popped up in reports to poison control centers and hospitals. Younger people or those with heart worries can end up in an ER with a dose no stronger than what’s sold online.
Somebody with a history of panic attacks, heart problems, or bipolar mood swings won’t get a warning label or a doctor at checkout. Mislabeling happens, dosages shift, and purity isn’t checked by the FDA. That’s not just fine print. A mix-up can send someone spiraling.
People like the idea that snacks or supplements can fix tough days. I get it. Life feels easier with a shortcut. But I’ve seen friends wind up jittery and sleepless from fuel drinks nobody questioned—and phenethylamine isn’t just a piece of chocolate. Supplement markets are quicker to hype than to test products. No one can easily promise phenethylamine is safe for everyone, every day.
If someone wants to feel better or sharper and hears about phenethylamine, it’s smarter to talk with a pharmacist or real-life doctor instead of trusting bright labels or slick marketing. Most of the evidence comes from tiny studies, not long-term use. Many antidepressants and ADHD medicines work much better, with careful oversight and checkups.
Better sleep, exercise, and eating foods that actually nourish you will do more than a new pill promising a brain boost. Trying out fads without guidance can backfire. It makes sense to question why something ends up on a shelf—and to push for more research before calling it safe.
Phenethylamine catches a lot of eyes, not just from chemists but from anyone looking for an extra mental boost. Some people refer to it as the “love drug” because of the similarity to the chemicals released during moments of happiness. You find it in chocolate, you see it in some supplements, and plenty of folks are curious about its potential mood-lifting effects. Looking at the bright side feels tempting, yet it’s worth pausing to examine the side effects that might tag along for the ride.
Reality hits pretty quickly once a person tries high doses of phenethylamine or takes it in concentrated supplement form. The head rush people chase after comes with some baggage. For starters, the body processes this substance quickly, which sometimes means effects come in waves—one moment you feel a boost, the next comes a crash. Jitters, anxiety, rapid heartbeat—those are just the familiar faces. Some people share stories about their blood pressure spiking or their hands turning clammy.
It’s not just the body that speaks up. For me, the feeling that follows isn’t always pleasant. There’s a tension that lingers at the edges, like having a little too much caffeine early in the morning, followed by an afternoon of sluggishness and frustration. A friend of mine tried it to get through a long day at work; instead of focus, he ended up feeling irritable and on edge, which only led to trouble in the break room.
Here’s the deal: phenethylamine acts like a stimulant. It ramps up the nervous system, making the heart work harder and signaling the brain to fire on all cylinders. For people already walking a tightrope with heart issues or blood pressure problems, this can create bigger trouble. There’s an even deeper ripple—high doses can bring on headaches, upset stomach, and, in stubborn cases, even paranoia or confusion. The risk grows if someone uses other substances that already speed things up, like certain antidepressants or over-the-counter cold meds.
Folks often bring up that “natural” label for comfort, but the body doesn’t really care where phenethylamine comes from once it’s inside. Just because chocolate has a pinch of it doesn’t mean a handful of capsules is a safe move.
People often chase a shortcut for energy, skipping meals and rest in favor of popping something that promises quick results. It’s easy to see the appeal—buying a bottle at the health store seems effortless compared to sorting out sleep or exercise. But using phenethylamine without understanding the risks puts both body and mind out of balance.
A more grounded approach means respecting the signals your body sends. Quick changes in mood, sweating with no clear cause, heart pounding—you don’t need a medical degree to know these are signs to slow down. Listening to people who’ve tried phenethylamine, patterns emerge: nearly every negative story could’ve been softened if they paid attention to these first signals.
Tossing caution aside for a fleeting high often brings more trouble than it’s worth. Phenethylamine isn’t some miracle molecule. The stakes rise for anyone stacking it with other drugs or ignoring warnings because they read something glowing on a forum. Doctors remain the best resource here—their job revolves around weighing risks and spotting trouble before it starts. Relying on experience, tuning into your body, and keeping communication open with professionals leads to fewer regrets and better health in the long run.
Phenethylamine, sometimes called PEA, has a reputation of being both fascinating and a little bit risky. The compound is found in chocolate and produced naturally in our brains, linked loosely with mood and alertness. People hear about it in the realm of mood enhancement or, on rare occasions, as a supplement for energy or focus. That sort of territory brings up the tough question: what counts as a recommended dosage?
PEA has been sold in capsules, marketed to improve mood or attention. The numbers that circulate usually land between 100 milligrams and 500 milligrams per serving. Some supplement bottles push for a whopping 500 milligrams, sometimes suggesting up to twice daily. On the other hand, mainstream research and chemical safety records tend to advise starting with much lower amounts—think 100 to 200 milligrams—and watching how the body reacts.
It’s easy to brush off milligrams as details that don’t matter, but real risks show up when the dosage jumps. PEA breaks down fast in the body thanks to the enzyme MAO-B, so taking it as-is doesn’t always guarantee wild effects. Pair it with other substances—especially anything that slows down MAO-B or combines with stimulants—and the results can get unpredictable. Blood pressure spikes, anxiety, heart palpitations, and headaches are no joke. Stories of people feeling jittery or panicked on doses that seemed “normal” highlight how quickly things can go wrong.
This isn’t fish oil or vitamin C. There’s an urge to chase more dramatic effects by upping the dosage, searching for those energetic highs. Chasing that with higher and higher doses brings the risk of overstimulation. I’ve seen friends experiment with all sorts of nootropics thinking they were harmless, then come to regret it after a sleepless night with a racing heart. What mainstream science does know is that PEA raises blood pressure and heart rate pretty noticeably, especially for people who already have some anxiety or heart issues.
Dosage advice in supplement communities is often passed around like folk wisdom, missing the context of individual health conditions. Some people experience sensitivity to stimulants. Anxiety disorders, high blood pressure, or medications that affect brain chemistry all play a big role in whether a “safe” dose actually is safe. The FDA hasn’t signed off on PEA supplements for medical use, and good clinical studies are thin on the ground. Companies that sell PEA rarely talk about these risks. Medical professionals tend to steer people away from it, or at least approach it with lots of caution.
Anyone considering this compound needs a grounded conversation with a doctor, especially if they have pre-existing health conditions or take any kind of psychiatric or blood pressure medication. Testing small, gradual increases under supervision rather than going for the higher recommendations on the label can prevent a nasty surprise. Being honest about why PEA is appealing goes a long way—if it’s about mood or focus, safer and more researched options probably exist. Keeping an open channel with a healthcare provider matters way more than chasing the promises of supplement advertising.
Phenethylamine, often called PEA, shows up in chocolate and gets produced naturally in the brain. It’s linked to energy, alertness, even feeling a bit happier. People can buy it in supplement form, usually chasing sharper focus or a lift in mood.
A lot of folks out there already know the routine: you find something promising, maybe PEA, and want to stack it with other stuff—caffeine, L-tyrosine, or even typical antidepressants. I’ve been down this road myself, wondering if mixing and matching could push things to the next level. It’s a fair question, but the reality is much less straightforward than health store labels or quick Google searches make it seem.
Most red flags pop up around prescription meds. Taking PEA with antidepressants, especially MAO inhibitors (MAOIs), can cause soaring blood pressure and a pounding heart. The reason: MAOIs slow the breakdown of compounds like PEA. This isn’t just theory—it’s a documented risk that’s landed people in the ER. Even everyday drugs, like some cold meds or stimulants for ADHD, may interact badly because they also deal with neurotransmitters. Once, a friend of mine tried mixing a focus supplement containing PEA with an ADHD prescription. Within hours, he felt jittery, his pulse raced, and his anxiety shot through the roof.
Looking at supplement combinations, the lines blur. You’ll see stacks sold online with PEA, caffeine, and amino acids like tyrosine or theanine. Some brands promise a bigger kick, better focus, or a longer mood boost. From chatting with users on forums and reading up on studies, the most common issues seem to be headaches, dizziness, or a sudden crash as the PEA wears off. Caffeine turns up the volume on these side effects, especially if you haven’t eaten. Some folks feel fine, but others end up too wired to concentrate or sleep. It’s tough to predict.
Labels aren’t everything. You don’t always know what’s in a supplement, much less how your body will handle multiple ingredients. I’ve learned that the best way to avoid surprises is to keep a health journal. Track what you take and how you feel. Small changes make a big difference. Even some herbal supplements, like St. John’s Wort, can shift how PEA and other drugs play together. These combinations haven’t been studied much, so guessing can be risky.
Before mixing PEA with anything, even a basic B-vitamin or a “natural” mood enhancer, talk to a doctor. Some pharmacists also know a lot about supplement-drug interactions—more than you might expect. For those committed to experimenting, start low, go slow, and keep track of every change. Online forums help, but remember that what works for one person could cause problems for someone else. Reliable information beats hype every time.
Curiosity drives the supplement market and everyone wants an edge. Mixing phenethylamine with other products or meds isn’t just a question of finding the right combo; it’s about recognizing that brains, bodies, and lives don’t all follow a script. Respecting that can mean the difference between a better day and a trip to urgent care.
| Names | |
| Preferred IUPAC name | 2-Phenylethan-1-amine |
| Other names |
PEA β-phenylethylamine 2-phenylethylamine phenylethylamine benzeneethanamine B-phenylethylamine |
| Pronunciation | /fiːˈniːθɪl.əˌmiːn/ |
| Identifiers | |
| CAS Number | 64-04-0 |
| 3D model (JSmol) | /3D/JSmol/MOL/58-08-2.mol |
| Beilstein Reference | 1209241 |
| ChEBI | CHEBI:4254 |
| ChEMBL | CHEMBL595 |
| ChemSpider | 986 |
| DrugBank | DB01482 |
| ECHA InfoCard | 100.003.387 |
| EC Number | 4.1.1.28 |
| Gmelin Reference | 62102 |
| KEGG | C06282 |
| MeSH | D010624 |
| PubChem CID | 1001 |
| RTECS number | SJ6000000 |
| UNII | X8ZC7V0N4I |
| UN number | UN2810 |
| Properties | |
| Chemical formula | C8H11N |
| Molar mass | 121.18 g/mol |
| Appearance | White to off-white crystalline solid |
| Odor | ammonia-like; fishy |
| Density | 0.964 g/cm³ |
| Solubility in water | Soluble |
| log P | 1.41 |
| Vapor pressure | 0.5 mmHg (at 25 °C) |
| Acidity (pKa) | 9.87 |
| Basicity (pKb) | 9.87 |
| Magnetic susceptibility (χ) | -75.0 × 10⁻⁶ cm³/mol |
| Refractive index (nD) | 1.528 |
| Viscosity | 0.963 cP (20 °C) |
| Dipole moment | 1.33 D |
| Thermochemistry | |
| Std molar entropy (S⦵298) | 340.6 J·mol⁻¹·K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | 93.7 kJ/mol |
| Std enthalpy of combustion (ΔcH⦵298) | –3732 kJ·mol⁻¹ |
| Pharmacology | |
| ATC code | N06BX18 |
| Hazards | |
| GHS labelling | GHS02, GHS07 |
| Pictograms | `COc1ccc(CCN)cc1` |
| Signal word | Warning |
| Hazard statements | H302, H312, H332 |
| Precautionary statements | P261, P264, P270, P271, P301+P312, P330, P405, P501 |
| NFPA 704 (fire diamond) | 2-3-0 |
| Flash point | 85 °C |
| Autoignition temperature | 595 °C |
| Explosive limits | Explosive limits: 1.1–6.6% (in air) |
| Lethal dose or concentration | LD50 (rat, oral): 820 mg/kg |
| LD50 (median dose) | LD50 (median dose) = 50 mg/kg (rat, intravenous) |
| NIOSH | SK1939000 |
| PEL (Permissible) | Not established |
| REL (Recommended) | 600 mg |
| IDLH (Immediate danger) | Unknown |